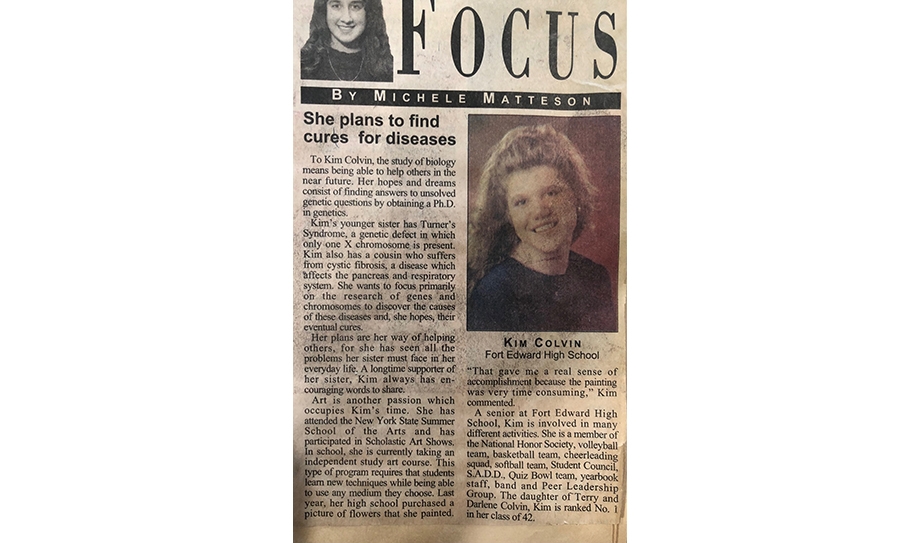
Kimberly A. Kelly’s small, hometown newspaper in upstate New York called it right years ago. They wrote that the brilliant and passionate then-high school student would one day find cures for diseases.
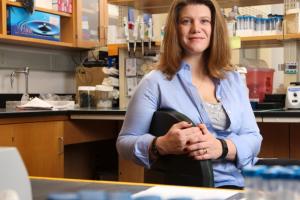
Today, Kelly, a University of Virginia biomedical engineering professor, is one step closer to fulfilling that prophesy. Kelly and her team at ZielBio Inc., the corporate offshoot of her research at UVA’s School of Engineering and Applied Science, have moved a potential cure for one of the world’s most heinous diseases into human clinical trials – a major step on the way to Federal Drug Administration approval.
Pancreatic cancer is one evil disease. Unfortunately, I know from experience. Before Christmas day dinner in 2016, I found my father stretched out on a couch in a quiet part of my parents’ home. His prized carving fork and knife lay beside him as he winced in abdominal pain. His grandkids a few rooms over were joyfully playing with their presents. Dad thought he must have eaten a bad oyster, part of a Tyree Christmas tradition, and tried to shake it off for the holidays, but the pain only intensified over the next few weeks. Soon after, his doctor called him and my mother into his office.
A pancreatic cancer diagnosis makes the floor fall out underneath you and the world grow black. They’d caught the disease early, his doctor said with controlled optimism, but the road ahead for Dad, and by extension, the family, would be pure agony.

Kelly has long understood the dire outcomes facing pancreatic cancer patients. She has made fighting the disease a focus for more than a decade.
The only current cure for pancreatic cancer is surgery, and only if the tumor has managed to stay around a small section of the pancreas that can be operated on—which occurs in about 20% of patients diagnosed with the disease, according to the American Society of Clinical Oncology. The five-year survival rate for people diagnosed with pancreatic cancer is less than 5%, mainly because symptoms don’t introduce themselves until the cancer has grown and spread, becoming inoperable.
In Dad’s case, even though they’d caught the cancer early, it was already so tangled around the head and body of the pancreas that surgery was no option. So, for almost the next two years, we watched helplessly as he shrunk into shivering bones – in no small part from the pain and the side effects associated with chemotherapy and radiation meant to slow the inevitable march of the disease.
Though pancreatic cancer kills only about 50,000 people a year in the United States, because of the vileness of the disease, hundreds of scientists around the world have been actively looking for ways to treat this cancer or provide a better quality of life for patients.
Among those at the top of this list is Kelly, whose breakthrough approach now offers hope that a more advanced treatment might be around the corner – one that would give pancreatic cancer patients, and by extension, patients with other types of cancers, the possibility of remission without the painful side effects of current treatments.

Kelly jokes that when she was a child, she thought her middle name was “Shut Up” because she tried her parents’ patience with constant questions. Eventually they ran out of answers and bought her a large book of explanations to mostly science-based inquiries, written for curious 8-year-olds. She’d get lost in those pages for hours.
“I just feel like I’m that child that never lost that curiosity, that wonder,” Kelly said. “I keep asking questions. And what my education has done is allow me to answer those questions with a sophisticated vocabulary.”
She also credits her high school art teacher and English teachers, Elizabeth and Dave O’Brien, for her accomplishments. “I think sometimes people don't understand that math and science are not just pragmatic, as in ‘this is what you do.’ They are absolute creativity. So, learning that creativity from the art world and from the writing world have really sparked all of this really cool experimentation and questions for me, that I can answer in new ways and push the technology. And that's where the intersection with engineering comes.”
Kelly’s eureka moment came in 2008 while she was an assistant professor of radiology at Massachusetts General Hospital. Using a technique known as phage display screening to identify peptides, short-chain amino acids which could be used as drugs for treating already known disease-related proteins on the surface of cells, she had an epiphany. What if she flipped the logic on its head?
“Drug manufacturers used phage display screening to find the drug. They already had the disease target in mind. But, I said, ‘Wait a minute. What if we could use this to find the disease target? What if we know the peptide identity and we put that on cells, like cancerous versus healthy cells, and let the peptides tell us what is different between them?’”
Those questions set her on her path of discovery. Kelly began developing a process she called ZielFind to discover and identify disease targets. ZielFind is unique in its approach in that the screening uses the live cellular context instead of an artificial environment used by other methods, which destroy the cell and lose important context like where proteins are located in the cell. In addition, ZielFind combines biology with computational methods to more accurately identify targets. This computational approach allows ZielBio to continuously collect data and efficiently and effectively apply their proprietary algorithms to zero in on targets.
“In the early iterations of ZielFind, you could only sequence about a hundred of those peptides, but there's billions of them. Now with next-generation sequencing, you can sequence through everything and then start comparing them statistically with bioinformatics and algorithms. So now when you do a screen, you can compare it to every screen we've ever done because we have these large databases,” Kelly said.
She was the first to find a protein called plectin sitting on the surface of pancreatic cancer cells. Plectin is normally found inside healthy mammalian cells, so this was an odd place for the protein to be hanging out. Plectin is known to stabilize cells structurally while essentially connecting junctions in the plasma membrane to other cells. In this way, plectin is a pivotal component in tissue integrity.
Shortly after the discovery of the plectin on the outside of pancreatic cells, and right before these results were published in 2008, Kelly joined UVA Engineering. Within months, she earned two National Institutes of Health grants to springboard her lab. Eventually, she formed a new company, ZielBio, to explore how to translate her discoveries into meaningful new therapies.
“Running a lab is very much like running a business. You must budget for personnel, you budget for supply, and you're making a five-year strategic plan in those grants. And it has to be exciting enough that 30 of your peers think, ‘Yeah, that's worth two and a half million dollars over five years. You are going to make an impact. We believe your data and you've done enough to convince us that you're really on that line between crazy and genius. You're not crazy. We're not sure if you're genius yet, but you're right there and it's worth the shot.’”
Since those early days, she’s taken one monumental step after another in her journey toward fulfilling her hometown newspaper’s prediction.
Why plectin sits on the top of pancreatic cancer cells is still a bit of a mystery, and one her team at ZielBio is investigating, but it was clear from their earlier research that plectin is key in the cancer’s metastasis and aggressive growth.
After they found that target, Kelly and her team of researchers at ZielBio were able to devise an antibody, ZB131, that only adheres to the plectin on the cancer cell surface and by doing that, it disrupts cancer functions. Because the antibody does not attack healthy cells, only the cancer cells, the hope is for minimal pain and other side effects for patients while their cancer is effectively treated.
Early lab results with ZB131 were so effective at shrinking, and even killing, pancreatic tumor cells that in late 2019, ZielBio announced it had secured $25 million in investor funding to launch the expensive process of bringing their patented, pancreatic cancer treatment to market and advance research into using their proprietary ZielFind method to find potential targets for other cancer treatments.
Kelly was able to leverage the resources available to UVA researchers to launch companies based on their research. Faculty entrepreneurship is a priority for the School of Engineering, which partners closely with the UVA Licensing & Ventures Group.
“Universities don’t have enough resources to actually bring these discoveries from labs to patients. It’s $25 million to take this one drug from a mouse antibody to a human antibody and then manufacture it,” she said. “But the University has been incredible all along the way. We initially worked with the Licensing & Ventures Group to investigate ways to commercialize our discoveries. We got a UVA-Coulter Translational Research Partnership award to explore leveraging plectin with an imaging agent and do an imaging clinical trial. We’ve had great support from Fred Epstein, biomedical engineering department chair, and Thomas Loughran, the UVA Cancer Center director. And we’ve had support from UVA’s Vice President for Research’s office.”

Despite the challenges many researchers faced during the COVID-19 pandemic, ZielBio has managed to hit all its necessary milestones and meet FDA requirements to progress to a phase 1/2 clinical research study.
The process of gaining FDA approval and bringing a drug to market is costly and time consuming for the very good reason of doing no harm. Once a lab has satisfied the FDA’s requirements for preclinical studies, such as Kelly’s lab did by testing ZB131 in mice, they can move into testing their drugs in humans.
The clinical trial part of the FDA approval process has three to four phases. Phase one involves testing in a small cohort of volunteer patients to determine dosage and safety. Phase two can include several hundred patients and focus on dosages, side effects and efficacy; phase three is similar to phase two but can include several thousand volunteers; After phase two or three, depending on the data, ZielBio can seek approval from the FDA. Just the phase 1/2 process often takes upward of two years to complete if everything goes according to plan.
At this point, the ZielBio team is focused on confirming safe dosages of ZB131 in humans. Working with a respected clinical research organization, ZielBio is conducting human trials at five sites nationally, including UVA Health.
Once ZielBio establishes that the drug is safe in humans and proper doses are dialed in, the team hopes by the end of 2022 to advance to the next phase of clinical trials with a larger cohort of patients, determining the drug’s efficacy compared to current standards of pancreatic, ovarian and bile duct cancer care.
“I honestly will cry if it helps one patient,” Kelly said. “It will be a lifetime achievement. I mean, honestly, it is very emotional.”
The experience of bringing an idea to market has also been a teachable moment for her students, who see Kelly not only as a professor but as someone who uses her creativity to make products that may go through the laborious and expensive process of FDA approval and eventually cure diseases.
“It is a great opportunity for UVA students to get educated on these things and then for ZielBio to have access to this talent,” Kelly said.
One of Kelly’s recent graduate students, Samantha Perez, has now signed on to ZielBio as a research scientist, where she will follow her scientific research into plectin and other new targets from Kelly’s lab into clinical studies in humans.
“The other thing that Samantha is really passionate about, and we are too at ZielBio, is health care equity and disparities,” Kelly said. “We want to figure out ways to partner with advocacy groups to bring our treatments to communities that are traditionally overlooked and underserved.”

Since Kelly’s initial discovery of plectin on pancreatic cells, she and her lab have found high levels of plectin on the surface of other cancers with high mortality rates: ovarian, lung, colorectal and Cholangiocarcinoma (bile duct cancer). She and her team are excited about the potential of ZB131 to treat other deadly cancers.
“Now that we're the first people to take this drug into the clinic against this new target, we are going to learn something. Do I think it will work? Absolutely. Might it work in the next nine months? We hope so. That's why we're doing this. Will we learn enough that if it doesn't work quite how we hoped, we can turn it around and make something else that will work? I believe so!”
My father would have been 75 years old this year. He would have been able to see my son graduate from high school in June. And if his diagnosis had come just five or six years later, perhaps he could have hoped to eventually benefit from Kelly’s advances.
Still, I’m very thankful for the research she and her team at ZielBio are doing to develop a treatment for pancreatic cancer. Like Kelly, I will be thrilled if ZielBio finds success and can help future patients and their families.
