People who are intubated for long periods of time — which has been the case for many serious COVID-19 patients — run the risk of pressure ulcers and other injuries to their airways from tubes inserted into their tracheas. The scarring that results can interfere with breathing, and surgery to remove the scar tissue often produces scarring of its own.
“Even before the pandemic, there were no good solutions to this problem,” said Donald Griffin, a biomaterials expert and assistant professor in the Department of Biomedical Engineering at the University of Virginia.
But a new approach being explored at the University of Virginia could bring the medical community closer to a solution.
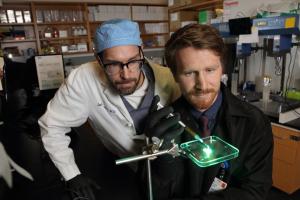
With funding from the National Institutes of Health, Griffin and his partner, James Daniero, a head and neck surgeon at UVA Health, will explore the use of a microporous annealed particle gel to promote healthy tissue growth after surgical intervention.
Injected into the incision, the gel would ideally serve as a scaffold for tissue regeneration, allowing the surrounding healthy tissue to infiltrate between the particles into gaps that are about the width of a human hair. The particles themselves would be resorbed as the tissue gradually knits together. One of the advantages to using a porous substance is that the body is less likely to reject it as a foreign body, as might be the case with a solid mass.
Employing a hydrogel to wounds in the trachea poses distinct challenges, but Griffin has cause for confidence. He has successfully applied this system to diabetic skin wounds, articular cartilage defect treatment and vocal fold reconstruction. His recent article on skin wound healing was featured on the cover of the April issue of Nature Materials.
“The space is really dynamic,” Griffin said. “People swallow, breath, cough and sneeze. The material has to adhere to the surrounding tissue and cohere to itself so that it doesn’t get worn away.”
Griffin will maximize adhesion and cohesion by using a mix of differently charged particles. The tissue that lines the larynx is negatively charged. For promoting adhesion, Griffin is relying on beads made from chitosan, a positively charged polymer commonly derived from shellfish.
“Chitosan has a collection of properties that are really useful,” Griffin said. “In addition to having a large positive charge, it is a coagulant, which makes it ideal to use after surgery.”
To encourage cohesion, Griffin has turned to chondroitin sulfate, the most common carbohydrate component of extracellular matrix tissue found in the larynx. Chondroitin sulfate has a negative charge, helping it hold the positively charged chitosan beads together.
Griffin’s challenge is to find the ideal proportion of chitosan and chondroitin sulfate to keep the scaffold as stable as possible and provide the best environment for wound healing. Using a microfluidic process that enables him to produce uniformly sized beads regardless of their chemistry, he will test various particle mixes in the laboratory for their mechanical strength and failure rate.
“I think somewhere in the middle, we will hit a composition with the greatest sticking power,” he said.
Griffin will then test the best-case particle mix in an animal model to confirm its stability under real-world conditions — as well as its ability to promote the regeneration of healthy tissue rather than fibrosis. At the same time, he hopes to use the opportunity to discover more about the biological processes that produce the new tissue.
Griffin emphasizes that if the project is successful, further refinements will be necessary before the treatment can be used in the clinic. He has a follow-on proposal to determine the optimal particle size for tissue growth.
“If the gaps between the particles are too large or too small, you will provoke an immune response,” he said. “The more we refine the platform, the closer we will come to having a translational therapy for a devastating condition that currently has no effective treatment.”
The researchers’ work is supported by the National Institutes of Health grant R21AR077163. Three years of funding from the UVA Coulter Translational Research Partnership provided a baseline for the team’s research on airway defects.