SelSym, a company co-founded by University of Virginia biomedical engineering professor Thomas Barker, is developing a product to stop uncontrolled bleeding caused by traumatic injury or surgery.
Findings published in April in Science Translational Medicine showed synthetic platelets made of ultrasoft hydrogel reduced bleeding in animal models.
The research suggests the technology could save lives as a transfusion alternative or point of care treatment if whole blood or platelets, cell fragments that help clotting, aren’t available when patients need them most — for example, on a battlefield or remote accident scene.
“You can’t do that with donated platelets because after about five days, they lose their function and may not be safe to use,” Barker said.
SelSym’s answer to the longevity problem, called SymClot, has already demonstrated a shelf life of six months at room temperature. The team members, including UVA research scientist Jagathpala Shetty and Barker’s co-founders and collaborators at North Carolina State University, Duke University and Chapman University in California, believe they can extend the window to one year.
In the face of blood shortages, the prospect has grabbed headlines in Wired and Fierce Biotech.

Special Molecules Boost Targeted Clotting
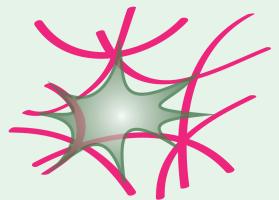
SymClot is composed of hydrogels, unique particles that are mostly water painted with special molecules designed to bind only to fibrin, a specific form of our natural blood-clotting protein found at wound sites.
The team calls the hydrogels “platelet-like particles” because they act like the real thing. Their properties turn up the clotting process where it is needed while allowing the particles to change shape, mimicking the behavior of natural platelets and leading to a process that enhances healing.
Even better, in the animal studies there appeared to be no “off-target” clotting and the particles were completely excreted by the kidneys. This suggests SymClot may be delivered into the blood stream to find and stop difficult-to-detect internal bleeding from traumatic injury.
In First Responders’ Hands
Next comes studies to support the team’s Food and Drug Administration application for the Investigational New Drug (IND) authorization needed to start human clinical trials, hopefully within two years.
“In another five years we could see this product in the hands of medics and doctors making an impact and saving lives,” Barker said. “It is exciting to think that SymClot could eventually be standard in basic first aid and trauma kits, further extending its impact to those in need.”
Before then, the technology must be scaled for manufacturing, which SelSym is working on with industry partners. While the hydrogel is easy to produce in quantity and quality, the team is investigating several approaches to scale production of the fibrin binding component in a cost-effective way.
The National Institutes of Health has granted SelSym about $3 million since the company’s founding in 2019, most of it for manufacturing feasibilities studies and preclinical research, according to Fierce Biotech.
Barker is a professor in the Department of Biomedical Engineering, a joint program of UVA’s School of Engineering and Applied Science and School of Medicine.