Researchers at the University of Virginia have discovered a new mechanism driving drug resistance in pancreatic ductal adenocarcinoma, one of the deadliest cancers. Their findings could lead to more effective treatments, providing hope for patients facing this aggressive disease.
Unveiling the Role of Hypoxia in Pancreatic Cancer Progression
Pancreatic tumors are notorious for their resistance to chemotherapy, due in part to their dense, poorly vascularized tissue structure, which creates areas of low oxygen, or hypoxia, within the tumor. Professor Matthew J. Lazzara, who holds appointments in the Department of Chemical Engineering and the Department of Biomedical Engineering, and his team from UVA Engineering set out to investigate how this hypoxic environment contributes to cancer cells becoming more aggressive and harder to treat.
“Our question was simple: Does the low-oxygen environment in pancreatic tumors drive cancer cells to become more resistant to chemotherapy? And if so, is this through the same pathways as those triggered by growth factors?” Lazzara said. Growth factors are naturally occurring proteins in the body that stimulate cell growth and survival. In cancer, they can also help tumors grow and evade treatments like chemotherapy by triggering changes that make cancer cells harder to destroy.
The team’s findings were striking. They showed that hypoxia indeed pushes pancreatic cancer cells into a more aggressive, chemoresistant state. However, the change triggered by low oxygen is far more durable than the similar effect caused by growth factors, making it a significant challenge for treatment.

A New Mechanism of Resistance
The study, published in Cancer Research, revealed that when pancreatic cancer cells are deprived of oxygen, a specific process is activated inside the cells. This process involves changes in the way the cells’ genetic material is modified and how signals are sent within the cell, making the cancer cells stronger and more resistant to chemotherapy. Unlike other changes caused by growth factors, this oxygen-deprivation-induced change is especially long-lasting — it can persist for weeks after the cells are exposed to low oxygen, making it more difficult to treat the cancer effectively.
“We found that once the cancer cells undergo this transition under hypoxic conditions, they become much more likely to resist chemotherapy. More importantly, we identified multiple ways to interrupt and even reverse this process,” said Brooke Brown, a collaborator on the study.
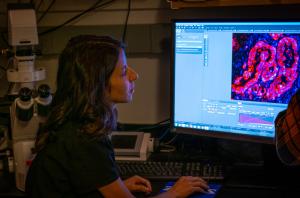
Using Innovative Techniques to Track Cancer Cells
To track the effects of hypoxia on pancreatic cancer cells, the researchers employed an innovative hypoxia lineage tracing system that was created by investigators at Johns Hopkins University. This allowed them to follow cells that had been exposed to low oxygen levels over time. Their findings were bolstered by data from multiple sources, including cell culture models, multiple mouse models and computational analysis of human patient data.
“This approach was new because we combined cell-based models, animal studies and computational analysis to comprehensively understand how hypoxia drives this chemoresistant state,” Lazzara said.
Implications for Future Treatment
The next steps for the team involve investigating how these pathways function in response to chemotherapy drugs, which are also known to drive similar resistance processes.
“We’re also exploring how hypoxia affects other cells in the tumor environment, such as fibroblasts,” Lazzara said.
This research represents a significant potential advance for pancreatic ductal adenocarcinoma treatment. The ability to disrupt the durable, hypoxia-induced changes in pancreatic cancer cells offers a potential breakthrough in improving patient outcomes. With new strategies that specifically target these resistant cancer cells, future therapies could be more effective at reducing tumor growth and combatting chemoresistance, leading to better survival rates for pancreatic cancer patients.
“Our findings highlight the importance of understanding the tumor microenvironment in developing new therapies,” Lazzara said. “By targeting the pathways that enable cancer cells to resist chemotherapy, we hope to bring new, more effective treatments to patients with pancreatic cancer.”
The study was supported by the National Institutes of Health and other key funding bodies and involved collaboration with researchers from the University of Pennsylvania and the University of Oulu, Finland.