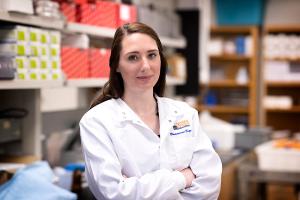
Rachel Bour discovered biomedical engineering, a combination of her two favorite subjects — biology and engineering — in high school.
Little did she know, a short time later she would be a Ph.D. student at the University of Virginia School of Engineering and Applied Science, instrumental in advancing the complex manufacturing processes needed to bio-print live muscle tissue. Bour is part of a team that’s getting closer to helping the thousands of American civilians and military personnel who suffer from permanent loss of skeletal muscle after injuries or diseases.
“I was exposed to the field of engineering from an early age, as both of my grandfathers were engineers,” Bour said. “I enjoyed creative problem-solving, and by high school, I knew I wanted to pursue engineering as a career. I liked the idea of engineering combined with biology because I could see how it could help individual people who were suffering from diseases or medical issues, but at a large, societal scale.”
She got research experience as an undergraduate at the Children's National Medical Center in Washington and as a research assistant at the University of Maryland School of Medicine after she graduated from the university there. She then joined top researchers at the UVA Center for Advanced Biomanufacturing, in the Department of Biomedical Engineering. She works with center founders George Christ, director and professor of biomedical engineering and orthopedic surgery for UVA’s schools of engineering and medicine, and Shayn Peirce-Cottler, professor of biomedical engineering, the David A. Harrison Distinguished Educator and graduate program director for the department.
The aim of the center is to promote the advancement of tissue engineering and regenerative medicine, especially supporting the translational part of the research lifecycle — the place where research is transformed into a product or a technology that can directly help patients. There is an urgency around this work because there are many medical situations, like those resulting from explosions during combat or birth defects like cleft lip palate, in which muscle and tissue are lost but cannot be regenerated and replaced by the body.
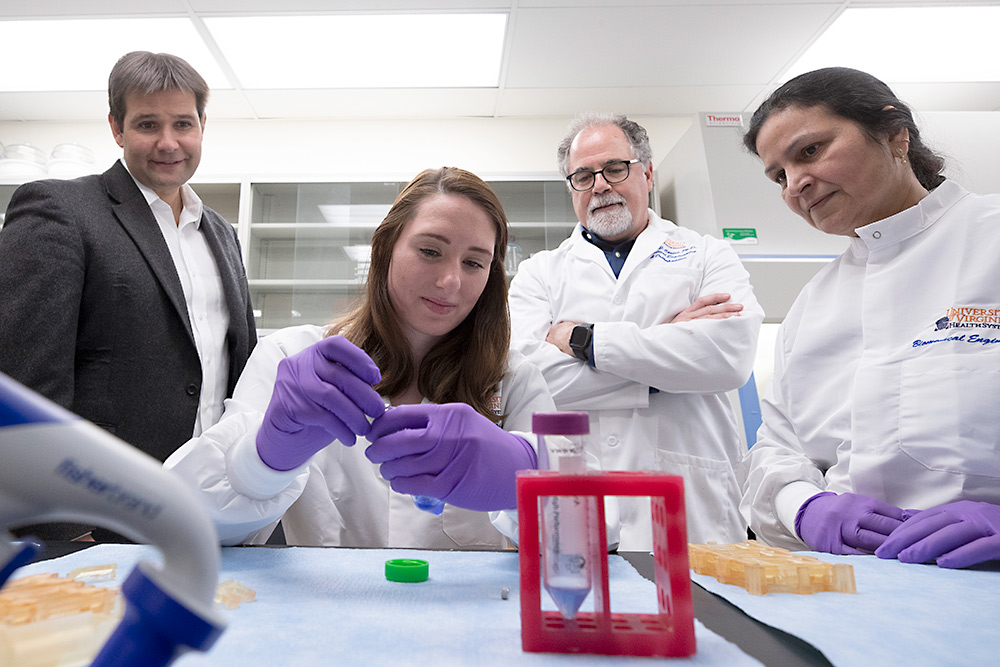
“With this new intersection of medicine and manufacturing, we are poised to bring new hope to patients who suffer from large-scale muscle loss,” said Christ.
Much of Bour’s research has focused on automating tissue-engineered muscle repair technology, or TEMR, developed by Christ.
The technology first involves obtaining muscle progenitor cells from a small portion of the patient’s muscle tissue. Muscle progenitor cells are descendants of stem cells and can differentiate into mature muscle cells. For her project, the patients are rats, but the technology has also been developed using human muscle cells from patient biopsies.
Bour then “grows” the skeletal muscle progenitor cells and seeds them onto a base-layer, called a scaffold, which is made of a pig bladder donated by Smithfield Biosciences.
“The scaffolds are mostly made of collagen. And since collagen is so well conserved among species, this material reduces the chance of eliciting an immune response from a rat or a human,” Bour said. “The body needs to accept the new tissue.”
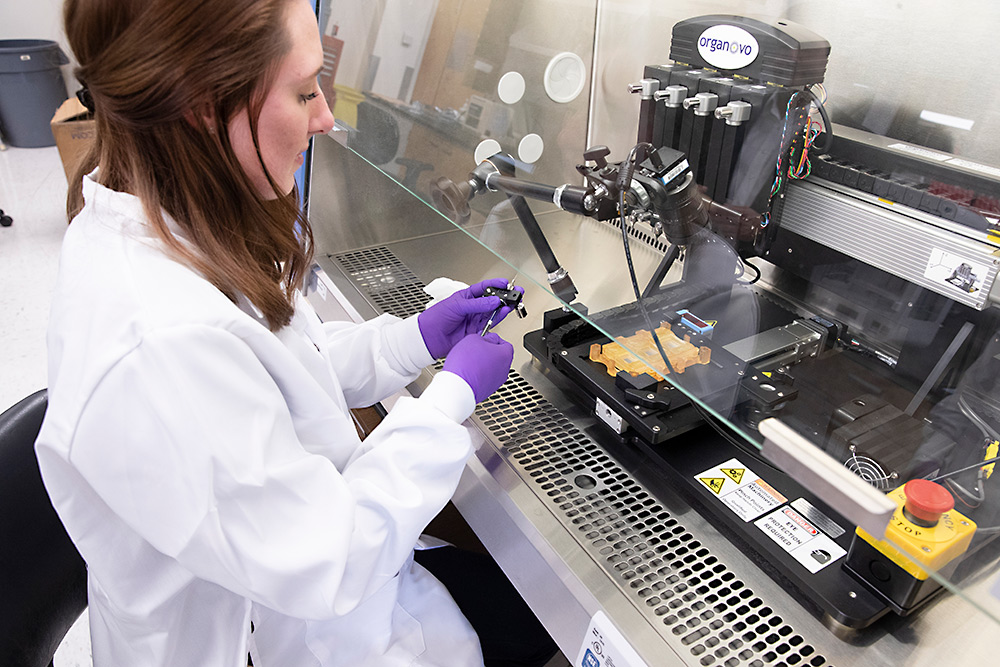
In the past, the scaffold needed to be hand-seeded with cells, but Bour has developed, along with lab manager Poonam Sharma, a way to automate the process by bioprinting cells in a single layer on the scaffold. She encapsulates the cells in a hyaluronic acid gel, a natural substance found in the body that acts as a cushion for tissue. She then uses an extrusion printer — a specialized 3D bioprinter — to print the cells onto the scaffold. Bour’s new method seats the cells more reliably, uses fewer cells and is more reproducible than hand-seeding.
Such innovations are critical for translating tissue engineering technology into help for patients, because automation enables production at large quantities and lower cost.
The next step in the process of making skeletal muscle tissue is putting a sheet of cells into something called a bioreactor. Together with associate professor Gavin Garner from the UVA Department of Mechanical and Aerospace Engineering, Bour has introduced some automation to this part of the process, too.
“In order to be ready to be placed into a living organism, the construct needs to be prepared in a special way.” Bour said. “The cells need to experience mechanical forces that help align and differentiate them.”
Bour and Garner worked together to eliminate the need for manual manipulation of the scaffold to create a fully enclosed bioreactor environment. The reactor now has holders that clamp down on the scaffold to hold it in place while it is exposed to stretching. The fully enclosed process does not need human intervention.
“At every step of the process, we are designing a more closed-loop system for manufacturing tissue, whether it’s creating automated and reproducible bioprinting methods or holders for the bioreactor,” Bour said.
“We hope one day to use robotic arms to move the developing tissue from one place to the next, like from the bioprinter to the bioreactor, so that no human intervention is needed to create the tissue from beginning to end.”
Bour is at the final stages of testing the engineered construct by placing it in rats. These trials will help Bour create critical quality attributes, a list of requirements and measurements that the finished product will need to prove reproducibility and potency. This is a crucial step necessary before moving toward solutions for humans.
Early results indicate that functional recovery in the rats’ muscles using the bio-printed process takes about one-third less time as compared to the hand-seeding method. This suggests that not only is the manufacturing process working, but also results in faster wound healing and repair.
Bour’s plans for her own career include working in industry, hopefully in the field of regenerative medicine. She was able to get industry experience during her doctorate when she earned a spot in the UVA Biotechnology Training Program, during which she did a three-month internship with the Advanced Regenerative Manufacturing Institute, a non-profit research organization dedicated to rapidly advancing biomanufacturing technologies.
The internship was closely aligned with her research at the UVA Center for Advanced Biomanufacturing. She connected with industry partners to help support the development of a tissue foundry — a closed-loop, automated manufacturing plant — and started scaling the bioreactor processes she developed so they could be included as part of the production line.
Bour’s experience with the training program was just what she hoped for.
“Besides working on a project that I knew would potentially help people, I really enjoyed the fast-paced environment of industry, with a whole team of people intently focusing on the same thing,” she said. “I liked the shared sense of purpose and the team spirit that comes with that.”
Bour’s work was made possible by a grant from the Advanced Regenerative Manufacturing Institute (ARMI/BioFabUSA) and the UVA Biotechnology Training Program.